Introduction
Malaria is a mosquito-borne infectious disease caused by single-celled microorganisms of the Plasmodium family. It is transmitted through the bite of virus-carrying female Anopheles mosquitoes. In tropical and subtropical areas, it is a serious worldwide health issue. It has a significant impact on millions of individuals globally and is a significant public health issue in many nations.
Several Plasmodium species are known to cause malaria in humans. Among them, Plasmodium falciparum is the most harmful since it can result in severe malaria and potentially lethal consequences.
Sub-Saharan Africa, as well as some regions of Asia, Latin America, and the Middle East, are among the regions of the world where malaria is most common. It is a terrible and occasionally fatal illness brought on by a parasite that frequently infects a particular species of mosquito that feeds on people. Depending on the area and the frequency of infected mosquitoes, different people are more likely to get malaria.
The condition is treatable and preventable with the right precautions, including mosquito control, prophylactic medication, and early diagnosis and treatment. Monitoring medication resistance, early diagnosis, timely treatment, and surveillance are other key components of malaria control strategies. Although there has been substantial success in malaria management, the disease still poses a threat to world health, and continued efforts are being made to prevent malaria.
Incidence
- The prevalence of malaria differs considerably between different parts of the world. The bulk of malaria cases and fatalities occur in sub-Saharan Africa, where malaria is most common in tropical and subtropical regions.
- An estimated 445,000 individuals died from malaria in 2016, the majority of whom were young children in sub-Saharan Africa. There was a reduction in malaria mortality by 25% between 2010 and 2016 and saved millions of lives globally, raising expectations and plans for elimination and ultimately eradication.
- Young people are the most vulnerable demographic in locations with high transmission rates.
- In 2016, it is thought to have resulted in 445,000 fatalities, 216 million clinical episodes, and an estimated 90% of deaths worldwide occurred in the WHO African Region.
- The estimates of the global burden of malaria provided by the World Health Organization (WHO) 2020 indicate that there were an estimated 241 million cases of malaria worldwide, resulting in roughly 627,000 fatalities. In 2021, nearly half of the world’s population was susceptible to malaria.
- Worldwide, there were reportedly 247 million cases of malaria in that year.
619 000 deaths from malaria were anticipated in 2021. - The WHO African Region bears a disproportionately large amount of malaria globally. 95% of malaria cases and 96% of malaria deaths occurred in the region in 2021. In the region, 80% of all malaria deaths were in children under the age of five.
Causes and Types of Malaria
Infection with parasites of the genus Plasmodium results in malaria. The following types are the most prevalent in humans:
Plasmodium falciparum
The bulk of malaria-related fatalities are caused by this species. Although it also occurs in other places, sub-Saharan Africa is where it is most common. It caused by the parasite P. falciparum can have serious side effects, including organ failure, anemia, and brain malaria.
Plasmodium vivax
This species is widely distributed and can be discovered in various regions of Asia, Latin America, and some regions of Africa. As the parasite can lay latent in the liver and reappear after some time, P. vivax might lead to recurrent cases of malaria. P. falciparum is more severe, although it can still have serious consequences.
Plasmodium malariae
This species, which is responsible for a less severe type of malaria, is widespread throughout the world. Infections with P. malariae can linger in the body for a very long time, and people may have symptoms sporadically over many years.
Plasmodium ovale
The distribution of the P. ovale is mostly in West Africa, where it is less widespread than other species. It can produce signs and symptoms resembling P. vivax malaria, such as recurrent attacks brought on by latent parasites in the liver.
Plasmodium knowlesi
This parasite can infect humans but predominantly affects non-human primates. It can cause severe and even fatal and is present in portions of Southeast Asia.
Risk Factors of Malaria
Several things can make someone more likely to have malaria. These risk elements consist of:
- Geographical distribution: Sub-Saharan Africa, where the bulk cases occur, is one of the tropical and subtropical regions with the highest rates of the disease. Exposure risk is increased when visiting or dwelling in regions with high malaria transmission.
- Mosquito exposure: Spending time outside in areas with Anopheles mosquitoes increases your risk of getting bitten and contracting an infection. Without the right safety precautions, activities like camping, trekking, or working in agricultural or forest regions might increase the danger.
- Time of day: The main malaria vectors, Anopheles mosquitoes, are often more active between twilight and dawn. Without taking precautions, being outside at these times can increase the danger of mosquito bites.
- Age and health: The infection and its sequelae are more likely to affect young children, pregnant women, and people with compromised immune systems, such as those with HIV/AIDS or receiving immunosuppressive therapy.
- Prior travel: Individuals may become infected with it if they move from a zone where the disease is not endemic to one where it is widely transmitted. Lack of information about preventative measures, such as applying insect repellents or taking antimalarial drugs, can further raise the risk.
- A lack of protective measures: Not utilizing insecticide-treated bed nets, not wearing protective clothes (such as long sleeves and pants), and not using insect repellents all increase the likelihood of being bitten by mosquitoes and contracting it.
- Medication resistance: The risk of treatment failure and side effects is increased in areas where specific strains of the parasite have developed medication resistance.
Incubation Period of Malaria
- The incubation period might vary based on the parasite species and unique host conditions, among other things.
- The incubation time for P. falciparum is normally between 7 and 14 days, though it can range from 5 to 21 days.
- The incubation period is typically longer for other Plasmodium species, such as P. vivax, P. ovale, and P. malariae.
- Relapses can happen in cases of P. vivax and P. ovale infections, and the duration can range from 10 days to several months.
Mode of Transmission of Malaria
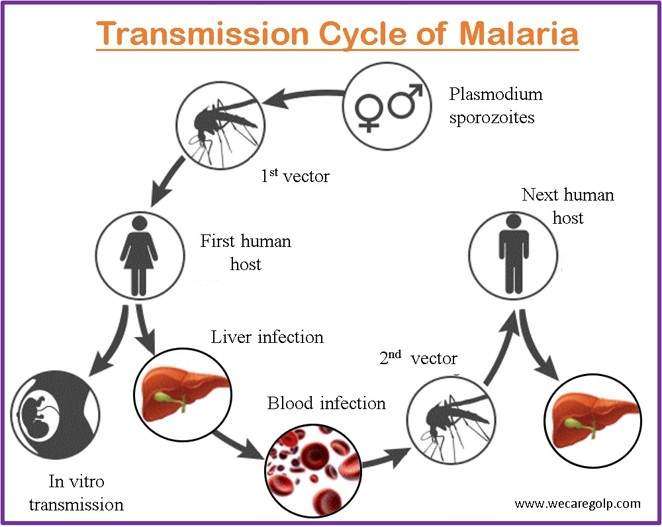
- Malaria is largely spread through the bite of female Anopheles mosquitoes carrying the infection. The malaria-causing Plasmodium parasites are ingested by mosquitoes when they bite a person who has the disease. The parasites are then introduced into the bloodstream along with the saliva when the infected mosquito bites another individual.
- It is also spread to the baby from an infected mother during pregnancy or delivery (congenital malaria).
- It may also be spread through blood transfusion, organ transplant, or the sharing of blood-contaminated needles or syringes because the parasite is found in the red blood cells (RBCs) of an infected individual.
Signs and Symptoms of Malaria
Depending on the type of malaria parasite involved, the person’s immune system, and the intensity of the illness, several signs and symptoms of malaria may appear. Malaria symptoms frequently manifest as:
- Fever: One of the defining signs of malaria is a fever. It may be intermittent, with periods of normal or slightly increased temperature interspersed with episodes of severe fever.
- Severe chills and sweats: Malaria patients may also have periods of intense chills followed by heavy sweating.
- Headache: Moderate to severe headaches, which may be throbbing or ongoing, might be brought on by malaria.
- Extreme tiredness and weakness: Malaria can cause severe fatigue and weakness, frequently accompanied by a lack of vitality.
- Muscle and joint pain: Malaria can induce generalized or localized muscle and joint pain, as well as body pains.
- Nausea and vomiting: Malaria patients occasionally experience nausea, vomiting, and appetite loss.
- Abdominal pain: Malaria can cause abdominal pain, discomfort, and diarrhea.
- Anemia: Malaria infections that are severe or prolonged can cause anemia, which manifests as a pale complexion, exhaustion, and shortness of breath.
- Jaundice: Malaria occasionally results in jaundice, a yellowing of the skin and eyes that indicates liver involvement.
- Modified mental status: Serious malaria infections, particularly those brought on by P. falciparum, can cause disorientation, impaired consciousness, convulsions, and coma.
Pathophysiology of Malaria
Humans and female Anopheles mosquitoes are cyclically infected during malaria’s natural history. The blood contains successive broods of parasites that grow inside the RBCs and decimate them, producing offspring parasites (“merozoites”) that continue the cycle by attacking other red cells. In humans, the parasites first grow and reproduce in the liver cells and subsequently in the RBCs of the blood.
The blood-stage parasites are what cause malaria symptoms; when specific types of blood-stage parasites (gametocytes, which come in both male and female forms) are ingested by a female Anopheles mosquito while blood-feeding, they reproduce in the mosquito’s gut and start a cycle of growth and multiplication. A parasite form known as a sporozoite migrates to the salivary glands of the mosquito after 10 to 18 days. As a result, the infected mosquito acts as a “vector” for the disease, while infected people pass on the parasite to the mosquito.
When the Anopheles mosquito takes a blood meal on another human, anticoagulant saliva is injected along with the sporozoites, which migrate to the liver and start a new cycle. The mosquito vector does not experience any negative effects from the parasites, in contrast to the human host.
Diagnosis of Malaria
Typically, a clinical evaluation, medical history, and laboratory tests are used to diagnose malaria.
The principal techniques for diagnosing malaria include:
Blood smear
The inspection of a blood smear under a microscope is the gold standard for diagnosing malaria. A qualified lab technician or healthcare practitioner applies a drop of the patient’s blood to a glass slide, lets it dry, and then examines it. To identify the species and stage of infection, they search for the presence of malaria parasites (Plasmodium species) and assess their characteristics.
Rapid diagnostic tests (RDTs)
RDTs are quick, easy tests that may be completed right away, even in settings with limited resources. A tiny blood sample is used to identify certain malaria antigens (proteins). RDTs can detect the presence of malaria and, in certain cases, the species of Plasmodium and can yield results in 15 to 20 minutes.
Polymerase chain reaction (PCR)
By amplifying the DNA or RNA of malaria parasites, PCR is a very sensitive molecular diagnostic tool. PCR can distinguish between several Plasmodium species and can find extremely small amounts of parasites in the blood. It is frequently employed for scientific research and in circumstances when precise species identification is important.
Other lab tests
The severity of the infection or the efficacy of the treatment may, in some situations, be determined by further laboratory testing like
- Complete blood count (CBC)
- Liver function test
- Renal function test
Treatment/Management of Malaria
Antimalarial drugs are frequently used in the treatment of malaria. The particular drug and treatment plan depends on several variables, including the type of malaria parasite involved, the affected organ, and the severity of the infection. Hospitalization is necessary if there is a medical emergency due to severe malaria. Here are some examples of frequently used antimalarial drugs:
- Artemisinin-based combination therapies (ACTs): For uncomplicated malaria caused by P. falciparum, the most prevalent and dangerous species of malaria, ACTs are the most effective and frequently advised antimalarial medications. ACTs combine a partner drug, such as lumefantrine or mefloquine, with an artemisinin derivative, such as artemether or artesunate.
- Chloroquine: In many regions of the world in the past, chloroquine was the first-line treatment for malaria, especially for illnesses brought on by P. vivax and P. ovale. Its use is now restricted to regions where the malaria parasite is still susceptible to the medication because of widespread drug resistance, particularly in P. falciparum.
- Alternative antimalarial drugs, such as atovaquone-proguanil, quinine, doxycycline, or clindamycin, may be administered in areas where certain strains of malaria are drug-resistant. Depending on the unique conditions and drug resistance trends in the area, these medications may be utilized as stand-alone therapies or in conjunction with other medications.
The severity of the infection affects the treatment options as well.
Complications of Malaria
Malaria can result in many consequences, especially if the infection is not identified and treated right away or if the person has underlying medical disorders. Malaria-related complications frequently include the following:
- Severe malaria: Malaria can sometimes develop into a severe form, especially if it is brought on by the P. falciparum parasite. Acute respiratory distress syndrome (ARDS), cerebral malaria (an infection of the brain), severe anemia, renal failure, liver dysfunction, and cardiac arrest are just a few of the problems that can arise from severe malaria. Severe malaria can be life-threatening and needs to be treated immediately.
- Organ dysfunction: Malaria can have an impact on a few body organs. If left untreated or if the infection persists, it can result in liver, kidney, and lung dysfunction and organ failure.
- Anemia: Malaria can significantly lower RBC levels, which results in anemia. Fatigue, weakness, shortness of breath, and other problems are all possible effects of severe anemia.
- Hypoglycemia: Low blood sugar levels (hypoglycemia) can occur in severe malaria infections, especially in youngsters. This may result in neurological issues such as seizures, unconsciousness, and more.
- Pregnancy complications: Malaria can be dangerous for both the mother and the fetus in pregnant women since they are more vulnerable to the infection. Pregnancy-related malaria complications include maternal anemia, low birth weight, preterm labor, and a higher risk of stillbirth or infant mortality.
- Recurrent infections: People who repeatedly contract the disease can develop recurrent cases of malaria in regions with significant malaria transmission. This may result in malaria-associated respiratory distress syndrome (MA-ARDS)
- Malaria-associated respiratory distress syndrome (MA-ARDS): MA-ARDS can appear in people with severe malaria. Intensive care management is necessary since it is characterized by significant lung damage and respiratory failure.
Prevention of Malaria
The following are effective malaria prevention measures:
Sleep under a bed net coated with insecticide (ITN)
- To prevent mosquito bites at night, when Anopheles mosquitoes, the malaria vectors, are most active, a physical barrier is made by bed nets, and mosquitoes are repelled and killed using an insecticide.
Indoor residual spraying (IRS)
- By routinely applying pesticides to the interior walls of homes, mosquitoes that come into contact with the surfaces are killed.
- In places with high transmission rates, this approach offers additional defense against malaria.
Mosquito avoidance
- It’s crucial to take precautions to keep mosquito bites at bay.
- Wear long sleeves, long pants, and socks, especially around dawn and twilight when mosquito activity is at its peak.
- Apply insect repellents as prescribed to exposed skin and reapply. Use clothing and equipment that has been permethrin-treated to ward off insects.
Antimalarial drugs (Chemoprophylaxis)
- If you’re going to a region where malaria is endemic, your doctor might recommend antimalarial drugs as a precaution.
- To suppress the parasites and avoid illness, these medications must be used before, during, and after travel, as advised for the particular destination.
Eliminate standing water
- By getting rid of places where mosquitoes breed, you can cut down on the number of mosquitoes. Cover or empty any containers, including buckets, flower pots.
Community-based interventions
- Community-wide initiatives can aid in reducing the spread of the infection.
- Larviciding (using larvicides to treat mosquito breeding grounds), environmental management, and community education about prevention, early symptom assessment, and rapid treatment-seeking behavior are a few of these.
Malaria vaccination
- The RTS/AS01 vaccine may be available and advised for specific age groups in particular regions.
- The vaccination offers some defense against P. falciparum malaria.
Travel advice
- If you are visiting a region where malaria is prevalent, learn about the specific malaria dangers and follow proper precautions.
- Take the advice of local health officials and travel medicine specialists.
Prognosis
- The type of malaria parasite, the patient’s general health, access to quick and efficient treatment, and any potential complications are only a few of the variables that affect the prognosis of malaria.
- It can be a serious and even fatal sickness, especially if left untreated or if the patient has underlying medical issues or a compromised immune system.
- The P. falciparum parasite may be lethal in extreme circumstances.
- It is vital to emphasize that the prognosis can vary depending on specific conditions, so it’s crucial to seek medical care right away if you think you may have the disease or if you reside in or have recently visited a region where the disease is endemic and have symptoms.
Summary
The Plasmodium parasite is the primary cause of the potentially fatal disease, which is mostly spread by the bite of infected female Anopheles mosquitoes. Tropical and subtropical areas, especially in sub-Saharan Africa, are prone to malaria. Fever, chills, headaches, muscle aches, exhaustion, and nausea are among the classic symptoms. In severe situations, it may result in potentially deadly complications such as organ failure, severe anemia, and brain malaria.
The diagnosis is made using a combination of clinical assessment and laboratory studies. It is treated by using antimalarial drugs. The specific treatment and regimen depend on elements such as the type of parasite, and the type of infection. Insecticide-treated bed nets, indoor residual insecticide spraying, wearing protective clothing and applying insect repellents to avoid being bitten by mosquitoes are some examples of preventive measures against malaria. The RTS-S/AS01 vaccine, which is only partially effective against P. falciparum malaria can be used as a preventive measure.
Read also:
References
- Buck, E., Finnigan, N.A. (2023, Jan 22). Malaria. StatPearls Publishing. Retrieved on 2023, May 18 from https://www.ncbi.nlm.nih.gov/books/NBK551711/
- Shahbodaghi, S. D., & Rathjen, N. A. (2022). Malaria: Prevention, Diagnosis, and Treatment. American family physician, 106(3), 270–278. PMID: 36126008. https://pubmed.ncbi.nlm.nih.gov/36126008/
- Zekar, L., Sharman, T. (2023, Jan). Plasmodium Falciparum Malaria. StatPearls Publishing. Retrieved on 2023, May 19 from https://www.ncbi.nlm.nih.gov/books/NBK555962/
- Center for Diseases control and Prevention. (2022, March 22). Malaria. Retrieved on 2023, May 19 from https://www.cdc.gov/malaria/about/faqs.html
- World Health Organization. (2023, March 29). Malaria. Retrieved on 2023, May 20 from https://www.who.int/news-room/fact-sheets/detail/malaria
- Milner, D. A., Jr (2018). Malaria Pathogenesis. Cold Spring Harbor perspectives in medicine, 8(1), a025569. https://doi.org/10.1101/cshperspect.a025569
- Jagannathan, P., & Kakuru, A. (2022). Malaria in 2022: Increasing challenges, cautious optimism. Nature communications, 13(1), 2678. https://doi.org/10.1038/s41467-022-30133-w