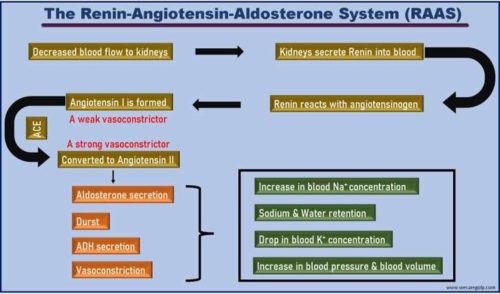
The Renin-Angiotensin-Aldosterone System (RAAS) is one of the most important physiological systems which plays a crucial role in controlling blood volume by regulating fluid and electrolyte balance. It involves many organs and hormones.
The Renin-Angiotensin-Aldosterone System (RAAS)
- The Renin-Angiotensin-Aldosterone System (RAAS) is a chief regulator that regulates blood pressure and water-electrolyte balance within the body on a long-term basis.
- In response to decreased renal blood flow, the main three hormones (renin, angiotensin II, and aldosterone) are responsible for the elevation of the arterial blood pressure.
- It provides a dynamic balance to maintain the homeostasis of the circulatory system.
Microscopic structure of the kidney
Nephron
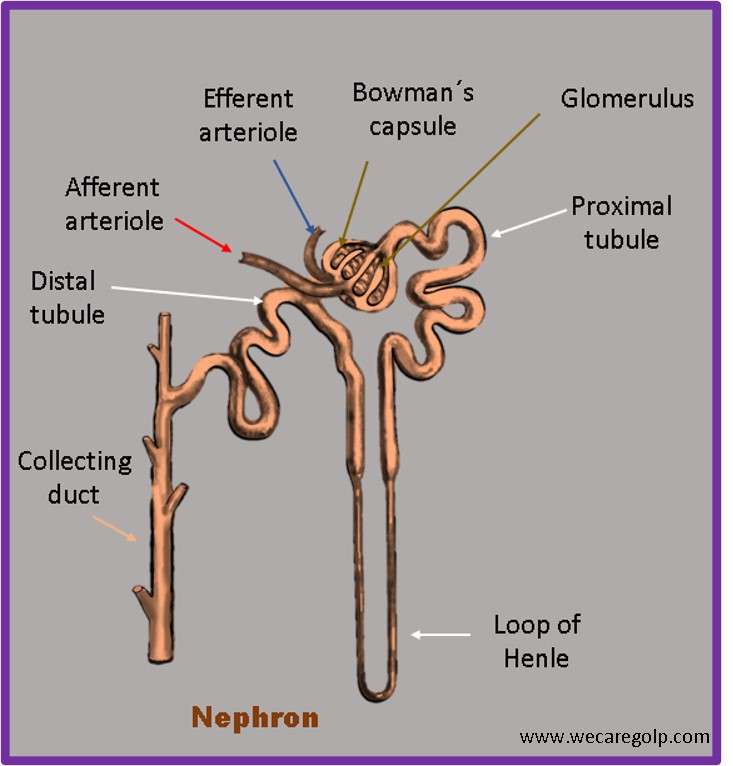
- Nephrons are the functional unit of the kidney.
- There are about 1.000.000 Nephrons in each human kidney
- Functions of Nephron:
- Formation of the primary urine (glomerular filtrate): in the renal corpuscles (180 L per day)
- Reabsorption of vital substances (e.g., calcium, potassium, sodium, glucose etc.)
- Formation of the secondary urine (terminal urine): in the tubular system (1.5 to 2.0 L per day)
- A nephron has two main components:
- Renal Corpuscles: Bowman´s Capsule with the Glomerulus
- Renal Tubules: Proximal Tubule, Loop of Henle & Distal Tubule
Juxtaglomerular Apparatus
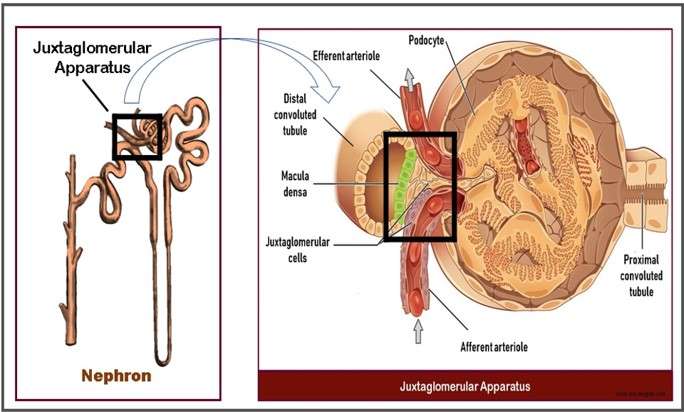
- The juxtaglomerular apparatus (JGA) is an anatomical structure in the nephron and formed by the afferent arteriole and the distal convoluted tubule of the same nephron.
- It is responsible for maintaining the renal as well as entire body volume status by regulating both intrarenal (glomerular filtration) and extrarenal (renin-angiotensin-aldosterone) mechanism.
- In the distal convoluted tubule, a group of specialized epithelial cells are present. These cells form macula densa and are sensitive to common salt (NaCl) concentration of the fluid in the tubule, more precisely chlorine ions. In response to decreased concentration of salt, the macula densa acts as a chemoreceptor and the enzyme renin is secreted.
Renin
- Renin is an enzyme which influences blood pressure.
- Additionally, its main task is to keep fluid volume in the circulatory system constant.
- Renin is synthesized from the granular cells of the juxtaglomerular apparatus of the nephron.
- The Renin-Angiotensin-Aldosterone-System (RAAS) is started by the release of renin.
When is renin produced?
- Decreased blood flow to the renal corpuscle
- Decreased in the amount of fluid that is filtered out in the renal corpuscles (decreased glomerular filtration rate- GFR)
- Decreased blood pressure in afferent arteriole, measured by the blood pressure sensors (baroreceptors)
- Decreased concentration of common salt (more precisely of Chlorine ions) in the distal convoluted tubule (measured by the salt sensors of the macula densa).
Mechanism of The Renin-Angiotensin-Aldosterone System (RAAS)
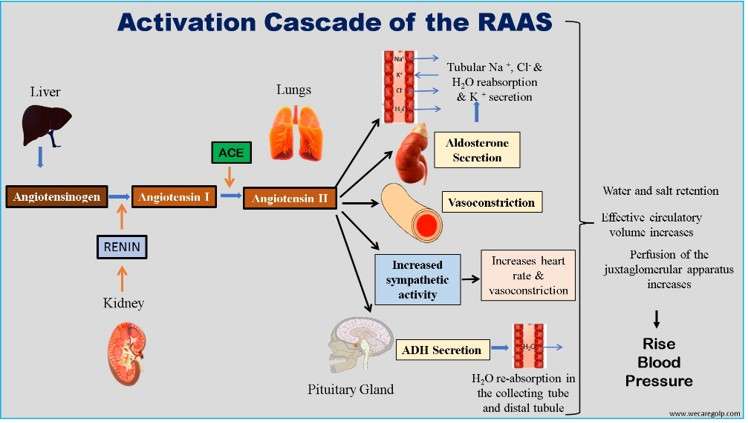
- The function of renin is to cleave angiotensinogen into angiotensin I.
- The angiotensin-converting enzymes (ACE) of the lungs and kidneys convert angiotensin I into angiotensin II. Angiotensin II is physiologically active.
- Angiotensin II is one of the most potent vasoconstrictors in the organism, causing an increase in peripheral vascular resistance and, thus, systemic blood pressure.
- On the other hand, it promotes aldosterone secretion in the adrenal cortex, resulting in increased sodium reabsorption and potassium secretion in the distal tubule.
Angiotensinogen
- Angiotensinogen (AGT) is a plasma protein from a group of serpins with vasoconstrictor effects.
- AGT has 485 amino acids and a molecular weight of 50 kD.
- It is synthesized in the liver and released into the bloodstream.
- Although AGT generally considers a passive substrate of the RAAS system, it is the most important and first component of this system that regulates blood pressure and body fluid.
- The enzyme renin converts the AGT into angiotensin I (decapeptide).
Angiotensin I
- The structure of Angiotensin I (Ang I) consists of ten amino acids (decapeptide). These are Aspartic acid (Asp), Arginine (Arg), Valine (Val), Tyrosine (Tyr), Isoleucine (Ile), Histidine (His), Proline (Pro), Phenylalanine (Phe), Histidine (His) and Leucine (Leu).
- It has biologically no direct function. However, high levels can stimulate catecholamine.
- When Ang I passes through the lungs, it is further converted into the octapeptide angiotensin II by another enzyme Angiotensin-Converting Enzyme (ACE).
- ACE is present mainly on the surface of the endothelial lining of pulmonary capillaries.
- ACE also causes the breakdown of bradykinin. Bradykinin is a vasodilator, whereas angiotensin-II is a vasoconstrictor.
Angiotensin II
- Angiotensin II (Ang II) is an octapeptide that forms by splitting off two amino acids (Histidine and Leucine) from angiotensin I under the action of angiotensin converting enzymes (ACE).
- Ang II is a biologically active and potent vasoconstrictor.
- Not only the breakdown of bradykinin (because of ACE) but also the effect of Ang II causes vasoconstriction, thus increasing blood pressure.
Functions of Angiotensin II
Correction of Electrolyte
- Ang II reabsorbs the sodium, chloride, and water and secrets the potassium on the tubule of the nephron. As a result, it maintains the fluid volume and blood pressure in the body.
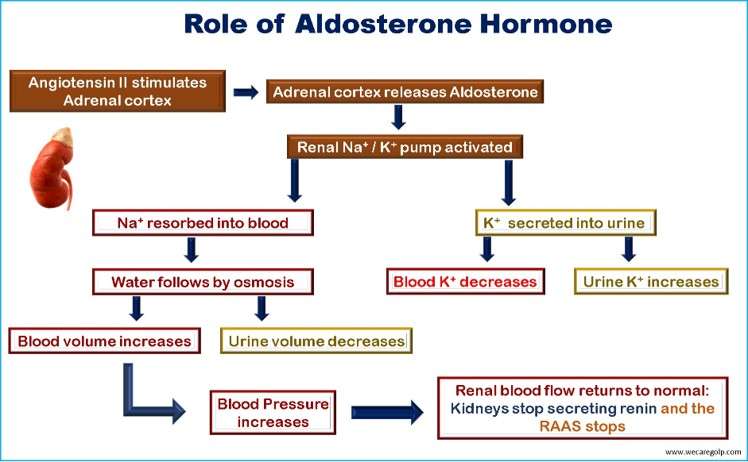
Secretion of Aldosterone
- Ang II stimulates the release of the hormone aldosterone from the adrenal gland.
- Aldosterone is a mineralocorticoid hormone.
- It promotes sodium and water reabsorption and potassium excretion in the distal convoluted tubule.
- The increased sodium concentration and fluid volume in the blood thus increase blood pressure.
Vasoconstriction
- Angiotensin II causes blood vessels to narrow (vasoconstriction), which increases blood pressure.
- The act of Ang II on receptors of venous smooth muscle leads to venous constriction. As a result, the cardiac output increases because of increased venous return. Hence the systolic blood pressure will also increase.
- Additionally, it influences cells of the smooth muscle of the artery and causes arteriolar constriction. Here, the diastolic blood pressure will increase due to the retention of blood and its pressure on the arterial side.
Stimulation of Sympathetic Nervous System
- Ang II increases the sympathetic activity in the central nervous system and secretes nor-epinephrine in the adrenal gland.
- Norepinephrine increases heart rate and also acts as a vasoconstrictor.
Release of Antidiuretic Hormone (ADH)
- At the same time, angiotensin II stimulates the production of Anti-diuretic Hormone (ADH) in the posterior pituitary gland.
- ADH, also called adiuretin or vasopressin, causes water re-absorption in the collecting tube and distal tubule.
- In addition, ADH (Vasopressin) also has a vasoconstrictive effect.
- In this way, ADH takes part in fluid and blood pressure regulation.
Summary
- In hypovolemia (e.g., due to fluid loss or insufficient fluid intake), sodium deficiency, or reduced renal perfusion, the RAAS is initiated by renin release.
- The synthesis of renin occurs in the juxtaglomerular apparatus.
- Its primary role is to prevent hypotension by stabilizing blood pressure, fluid volume, and sodium and potassium balance.
- Renin cleaves a peptide (Angiotensin I) from angiotensinogen produced in the liver.
- Angiotensin I is converted into angiotensin II by the enzyme ACE produced in the lungs.
- In conclusion, the volume expansion (via aldosterone and ADH) and increased peripheral vascular resistance (via angiotensin II and vasopressin) regulate gradually blood pressure for a long period.