Introduction
Filariasis, also called lymphatic filariasis, is a parasitic disease, brought on by an infection with filarial worms. Worldwide, millions of individuals living in tropical and subtropical areas are afflicted with filariasis. Lymphatic filariasis, a neglected tropical illness, is also called elephantiasis. Humans contract filariasis from the bite of infected mosquitoes, especially those from the genera Anopheles, Culex, and Aedes. Chronic infection can result in swelling of the extremities, hydroceles, and testicular tumors.
The lymphatic system suffers concealed harm from an infection, which is typically acquired throughout childhood. The three primary species of filarial worms infect humans and lead to sickness. The most prevalent species, Wuchereria bancrofti, is responsible for the most of cases worldwide. Depending on the stage of the infection, filariasis can result in a variety of clinical symptoms such as skin rashes and pain in the affected limb.
To eradicate this disease, the Global Programme to Eliminate Lymphatic Filariasis (GPELF) offers mass drug administration (MDA) to populations in endemic areas. The main goals of filariasis prevention strategies are the use of protective gear and mosquito control. To lower the number of microfilariae circulating in communities and to break the cycle of transmission, antiparasitic drugs have been distributed to individuals at-risk in endemic areas through MDA programs.
Incidence
- According to World Health Organization (WHO), most filariasis occurs in tropical and subtropical regions, with an estimated 800 million individuals at risk of infection.
- More than 80 nations have endemic cases of the illness, mostly in Africa, Asia, the Western Pacific, and parts of the Americas.
- As of 2018, there were 51 million cases of filariasis. This number has fallen by 74% since the WHO started GPELF in 2000.
- Due to the effective implementation of the WHO policies, 692 million individuals no longer need preventative chemotherapy.
- Some countries like Congo, Bangladesh, Nigeria, India, and Indonesia have the greatest prevalence of filariasis.
- In some areas, MDA initiatives have been effective in lowering the incidence and prevalence of the illness. These programs distribute antiparasitic drugs to at-risk groups.
Incubation Period of Filariasis
The incubation time can vary between 8 to 16 months, although it can also be as little as 4 weeks.
Causes of Filariasis
- The three primary types of filarial worms which are responsible for causing filariasis are
- Wuchereria bancrofti,
- Brugia malayi, and
- Brugia timori
- These parasitic worms are spread to people by the bite of infected mosquitoes, primarily those of the genera Anopheles, Culex, and Aedes.
Risk Factors of Filariasis
There are several risk factors for contracting filariasis such as:
Geographical location
- Filariasis is most common in tropical and subtropical areas.
- Being exposed to infected mosquitoes, for example, when living or traveling in places where the disease is common, raises the likelihood of an infection.
Exposure to mosquitoes
- The risk of infection rises with repeated mosquito bites, especially those from species that are known to spread filarial worms.
- Those who reside in or frequently visit locations with a high mosquito population and insufficient mosquito control methods are more vulnerable.
Poor sanitation and water management
- Filariasis transmission can be worsened in regions with subpar sanitation and bad water management.
- Stagnant areas of water provide a habitat for breeding mosquitoes.
Limited access to healthcare and poverty
- Filariasis is regarded as a disease of poverty.
- The persistence and spread of filariasis in impacted populations can be attributed to a lack of access to healthcare services, including preventive measures like mosquito control and antiparasitic drugs.
Occupation and lifestyle
- People engaged in outdoor, construction, or agricultural activities may be more exposed because of their surroundings at work.
- People who sleep outside or spend time in places with a lot of mosquitoes are at a higher risk.
Immune system weakness
- People with weak immune systems, such as those who have HIV/AIDS or other immune deficiency diseases, may be more susceptible to infection.
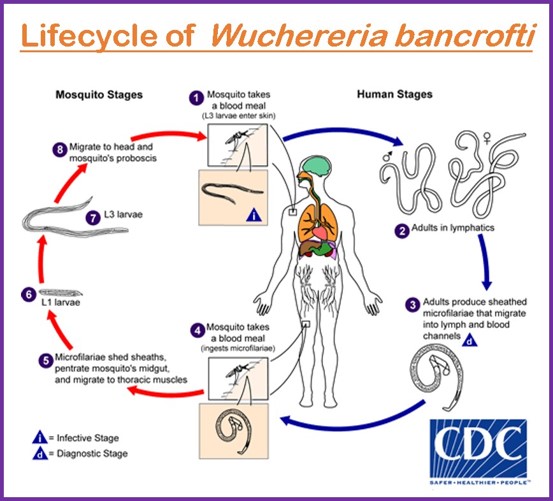
Mode of Transmission of Filariasis
- The primary way of transmission for filariasis is by mosquito bite.
- The filarial worms that spread the disease complete a portion of their life cycle in the mosquitoes that carry them.
Signs and Symptoms of Filariasis
In some situations, the infection’s first stages may be accompanied by acute symptoms.
- Fever
- lymphadenitis (inflammation of the lymph nodes),
- lymphangitis (inflammation of the lymphatic vessels),
- Skin rashes
- Pain in the affected limbs
- Acute bouts may sporadically recur.
Chronic filariasis is defined as chronic lymphatic dysfunction brought on by long-term, gradual damage to the lymphatic system.
Pathophysiology of Filariasis
A human bitten by an infected mosquito will have immature larvae (called microfilariae) injected into their circulation. These microfilariae move to the lymphatic system, where they continue to grow. The lymphatic system is the primary organ attacked by filarial worms. They move through the lymphatic channels before arriving at the lymph nodes and settling there.
The microfilariae grow into adult worms in the lymph nodes. Female worms discharge microfilariae into the circulation, lymphatic channels, or other body fluids after mating with the male worms. By doing so, the life cycle is maintained, and mosquitoes can transmit the disease while feeding on blood.
Immunological response in the host is brought on by the presence of filarial worms. The immunological response could be weak at first, allowing the worms to take hold. Immune cells, including eosinophils, lymphocytes, and macrophages, are activated by the immune system in response to the presence of the worms and their antigens.
The damaged tissues experience chronic inflammation as a result of the inflammatory mediators released by these cells, including cytokines and chemokines. Persistent inflammation and tissue damage in the lymphatic system can result in lymphatic dysfunction. Lymphatic dysfunction hampers the natural movement of lymph fluid, which can result in lymphedema (swelling), lymphangitis (inflammation of the lymphatic vessels), and other problems.
Chronic inflammation and prolonged exposure to filarial antigens can cause tissue remodeling and fibrosis (excessive scar tissue formation). Fibrosis can worsen lymphatic dysfunction and further clog lymphatic channels, which can lead to the severe skin changes.
Diagnosis of Filariasis
Clinical evaluation, laboratory tests, and imaging studies are frequently used to diagnose filariasis. The following are commonly employed filariasis diagnostic techniques:
Clinical evaluation
- Vital information for the diagnosis of filariasis can be gleaned from a comprehensive medical history and physical examination.
- Filariasis may be suspected if there are signs like limb enlargement (lymphedema), hydrocele, chyluria, or recurrent fever episodes.
- The patient’s travel history to endemic areas and exposure to mosquito bites should also be evaluated.
Blood microscopy
- One of the most popular ways to diagnose filariasis is through microscopic analysis of blood samples.
- Due to the microfilariae’s nocturnal periodicity, the blood samples are normally taken at night or in the evening.
- The preparation, staining, and analysis of a thick or thin blood smear are examined under a microscope to identify and characterize the microfilariae.
Antigen detection tests
- These tests can be used to identify blood-circulating filarial antigens.
- It can identify the presence of mature filarial worms and is very sensitive and specific. In determining the presence of a W. bancrofti infection, they are especially helpful.
- The immunochromatographic test (ICT) and enzyme-linked immunosorbent assay (ELISA) are two examples of antigen detection tests.
Polymerase chain reaction (PCR)
- PCR-based approaches can find and isolate filarial DNA in blood samples.
- PCR is incredibly sensitive and can find very small amounts of infection. It can be utilized to distinguish between current infection and previous exposure and identify the types of filarial worms.
- PCR is a very useful tool for reference and research labs.
Imaging studies
- The degree of lymphatic damage in people with chronic filariasis can be evaluated using imaging techniques like ultrasonography or lymphoscintigraphy.
- While lymphoscintigraphy includes injecting a radioactive tracer to evaluate the lymphatic system’s performance and identify any blockages or abnormalities, ultrasound can help show lymphatic abnormalities like dilated lymphatic channels.
Serological test
- It isused to find antibodies that the host produces in response to filarial infections.
- These assays are frequently employed in research settings or to establish previous filarial worm exposure.
- Enzyme immunoassays (EIAs), a type of serological test, may not be able to distinguish between several species of filarial worms and are not specific for detecting active infection.
Treatment/Management of Filariasis
The goals of filariasis management and treatment are to lessen symptoms, stop the spread of the disease, and stop transmission. The strategy can include medication therapy, symptom management, and preventative actions.
Drug treatment
Antiparasitic drugs are used as the main form of treatment for filariasis to eradicate adult worms and/or prevent the development of microfilariae. The particular treatment regimen is determined by the type of filarial worm and the clinical manifestation.
Drugs that are frequently used include:
- Diethylcarbamazine (DEC): This medication is the first choice for treating lymphatic filariasis brought on by B. malayi and W. bancrofti. DEC eliminates microfilariae and lowers the population of adult worms.
- Ivermectin: Ivermectin has demonstrated effectiveness in treating lymphatic filariasis brought on by W. bancrofti and Onchocerca volvulus when paired with DEC or used in combination with albendazole.
- Albendazole: For the treatment of lymphatic filariasis, it is frequently combined with DEC or ivermectin. Albendazole may have an impact on adult worms in addition to assisting in the reduction of microfilarial density.
Symptomatic management
Symptomatic treatment is essential for those with chronic filariasis and related symptoms, including lymphedema, hydrocele, or chyluria, to improve the quality of life. Symptom control options include:
- Elevation and compression therapy: Using compression bandages or garments and elevating the affected limbs can help reduce edema and enhance lymphatic drainage.
- Physical therapy: To encourage lymphatic drainage, reduce swelling, and improve mobility, exercises, massages, and manual lymphatic drainage techniques may be advised.
Surgical interventions
In some situations, it may be necessary to consider undergoing surgery to treat consequences like hydrocele or severe lymphedema. Surgical procedures can reduce discomfort and enhance function.
Complications
Particularly in people with recurring or protracted infections, filariasis can result in several problems. These problems may affect multiple body systems including:
- Lymphedema
- Hydrocele
- Chyluria
- TPE (tropical pulmonary eosinophilia)
- Primary (bacterial) and secondary infections: Cellulitis, abscesses, and fungal infections (might result in further problems and morbidity)
- Impaired immunological function
- Social Stigma and Psychological Impact
Prevention of Filariasis
The incidence and spread of filariasis can be significantly decreased through prevention. The following precautions are crucial for containing and halting the disease’s spread:
Control of vectors
- Utilizing bed nets: People can avoid mosquito bites by sleeping under insecticide-treated bed nets, especially at night when filarial mosquitoes are most active.
- Spraying pesticides inside homes can help repel or eradicate mosquitoes, thereby lowering their presence inside. This method is known as “indoor residual spraying.
- Environmental management: It is crucial to get rid of mosquito breeding grounds. This includes
- Eliminating standing water sources where mosquitoes grow,
- Making sure suitable drainage and sewage systems are in place, and
- Disposing of solid waste properly.
Personal safety precautions
- Use insect repellents: Spraying clothes and exposed skin with a repellent can help prevent mosquito bites.
- Use protective clothes: Long sleeves, long pants, and socks can act as a physical deterrent to mosquito bites.
- Limit outdoor activities at dusk and dawn: During these times, mosquitoes that spread filariasis are most active.
Mass drug administration (MDA)
- MDA programs distribute antiparasitic drugs to entire communities or at-risk groups, regardless of each recipient’s level of infection.
- This strategy attempts to cure sick people, lower microfilariae levels, and stop filarial worm transmission.
Health education and community engagement
- It is important to run public awareness programs to inform people about filariasis, how it spreads, and how to prevent it.
- This includes highlighting the significance of taking personal safety precautions, using bed nets, and taking part in MDA activities.
Surveillance and monitoring
- Regular surveillance and monitoring of the incidence of filariasis, mosquito populations, and treatment uptake are crucial for assessing the success of control initiatives, pinpointing hotspots of transmission, and directing intervention measures.
Integrated approach
- Combining the fight against filariasis with other disease prevention initiatives, such as those aimed at eradicating malaria or other neglected tropical diseases, can result in more effective and affordable interventions.
Prognosis
- The prognosis of filariasis depends on different variables such as the type of parasite, the extent of the infection, and the patient’s immunological response. In addition, early detection, the right course of action, and efficient symptom and complication management also influence its prognosis.
- If a person is not treated after contracting filariasis, it can last for years as a chronic disease.
- Over time, symptoms and problems may become more severe.
- The quality of life of infected persons can be enhanced with prompt intervention, which can also decrease the disease’s progression.
- The prognosis could be worse in extreme patients with advanced problems.
Summary
Filariasis is a chronic illness mostly affecting the lymphatic system that is brought on by parasitic worms. Not everyone infected with filarial worms exhibits symptoms. Some infected people may remain asymptomatic for years. There are effective treatments and management options, including medicines like diethylcarbamazine and ivermectin. An early diagnosis and action can stop the progression of a disease and enhance the quality of life.
With a correct diagnosis, an appropriate treatment, and management, the severity of the disease can be diminished. If the infection is not treated, it can last for years while also worsening in terms of symptoms and implications. Complications may include lymphedema and hydrocele, while symptoms may include swelling, pain, and skin issues. Control initiatives aim to minimize transmission through mass medicine administration, mosquito control, and improved sanitation.
Read also:
References
- Newman, T.E., Juergens, A.L.(2023, Feb 5). Filariasis. StatPearls Publishing. Retrieved on 2023, May 30 from https://www.ncbi.nlm.nih.gov/books/NBK556012/
- Lourens, G. B., & Ferrell, D. K. (2019). Lymphatic Filariasis. The Nursing clinics of North America, 54(2), 181–192. https://doi.org/10.1016/j.cnur.2019.02.007
- Medeiros, Z. M., Vieira, A. V. B., Xavier, A. T., Bezerra, G. S. N., Lopes, M. F. C., Bonfim, C. V., & Aguiar-Santos, A. M. (2021). Lymphatic Filariasis: A Systematic Review on Morbidity and Its Repercussions in Countries in the Americas. International journal of environmental research and public health, 19(1), 316. https://doi.org/10.3390/ijerph19010316
- Center for Diseases control and Prevention. (2018, October 22). Parasites Lymphatic Filariasis. Retrieved on 2023, May 30 from https://www.cdc.gov/parasites/lymphaticfilariasis/index.html
- World Health Organization (2022, March 16). Lymphatic Filariasis. Retrieved on 2023, May 29 from https://www.who.int/news-room/fact-sheets/detail/lymphatic-filariasis.
- Mathew, C. G., Bettis, A. A., Chu, B. K., English, M., Ottesen, E. A., Bradley, M. H., & Turner, H. C. (2020). The health and economic burdens of lymphatic filariasis prior to mass drug administration programs. Clinical Infectious Diseases, 70(12), 2561-2567. DOI: 10.1093/cid/ciz671
- King, C. L., Suamani, J., Sanuku, N., Cheng, Y. C., Satofan, S., Mancuso, B., … & Kazura, J. W. (2018). A trial of a triple-drug treatment for lymphatic filariasis. New England Journal of Medicine, 379(19), 1801-1810. DOI: 10.1056/NEJMoa1706854