Introduction
Measles (Rubeola) is a highly contagious viral respiratory illness caused by the measles virus, the single-stranded, linear, negative-sense RNA virus, that belongs to the family Paramyxoviridae, a member of the genus Morbillivirus. It is an acute febrile viral illness that can be prevented and causes rashes all over the body. It can be transmitted between humans directly through contact with sick people or through respiratory droplets.
- It is one of the most infectious illnesses, that can spread to vulnerable home contacts through secondary infections at a rate of at least 90%.
- Children are more likely than adults to contract the virus. Yet, anyone can have it at any age.
- Infections can permanently confer immunity.
- It still contributes significantly to worldwide mortality and morbidity.
- Most patients recover fully after treatment; however, there are very rare circumstances in which a patient may become ill, experience health issues, or even pass away.
- Particularly, people with weakened or insufficient cellular immunity may experience severe forms with non-pathognomonic clinical characteristics.
- Those undergoing chemotherapy for cancer
- Receiving organ transplants
- Suffering from AIDS
- Those with any type of congenital immunodeficiency
- Measles outbreaks can lead to epidemics that result in numerous fatalities, particularly in young, undernourished children.
- The best method of protection from infection is measles vaccination.
- Although antiviral may be necessary for certain individuals, supportive care is used to handle most cases.
Incidence
- Epidemiology varies globally and is influenced by the level of immunization attained in a certain area.
- Before major vaccination campaigns, an estimated 2.6 million people died from measles.
- The WHO projected that there were approximately 353,236 measles cases worldwide in 2018. Since then, this has dropped, as there were approximately 159,000 instances in 2020.
- In the United States, deaths from measles were documented in 0.2% of cases between 1985 and 1992.
- According to the World Health Organization (WHO), around 134,200 deaths occurred in 2015.
- The CDC reports that there were 372 cases in 2018 and 764 cases as of May 2019. In 2018, there were over 140 000 measles-related deaths worldwide, with the majority of those deaths occurring in children under the age of five.
- Measles vaccination caused a 73% decrease in measles mortality globally between 2000 and 2018.
Incubation period
- It has an incubation period of 10 to 14 days, starting four days before the rash appears and ending four days afterward.
- The greater intensity of the coughing coryza phase, which is accompanied by high viremia levels, favors the spread of viruses by droplets.
Causes of Measles
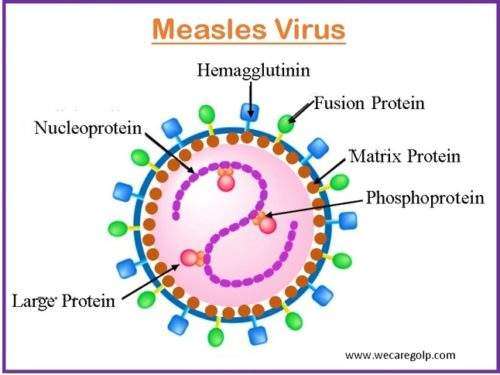
- The measles virus, a single-stranded, negative-sense enveloped RNA virus belonging to the genus Morbillivirus and family Paramyxoviridae, causes the disease.
Risk Factors of Measles
- Not getting the necessary vaccinations
- Missing the second vaccination dosage
- Visit endemic regions.
- Contact with tourists from endemic regions
- Immunodeficiency
- Malnutrition
- Pregnancy
- Vitamin A Deficiency
- Age of less than five years or greater than twenty years.
Mode of Transmission of Measles
- Direct- Droplet Transmission
- Indirect-airborne Transmission
- Other aerosol droplets and respiratory secretions, which are contagious for several hours, help disseminate the virus through the respiratory system. Upper respiratory tract or conjunctival contact is required to contract the infection.
- In addition to small particle aerosols that linger suspended in the air for several hours, respiratory droplets that travel short distances can transmit the measles virus.
Signs and Symptoms of Measles
High Fever
- Frequently >104°F (40°C)
- Fever lasts 4–7 days
Prodromal phase
- The 3 Cs
- Conjunctivitis (pink or red eye)
- Cough
- Coryza (fever, head cold, sneezing)
- Malaise
- Anorexia
Koplik spots

- Koplik spots are small, white patches on the bright red buccal mucosa that occur on the inside of the cheeks.
- They are thought to be specific to measles.
- It appears 1–2 days before the rash or during the prodromal stage.
Exanthem
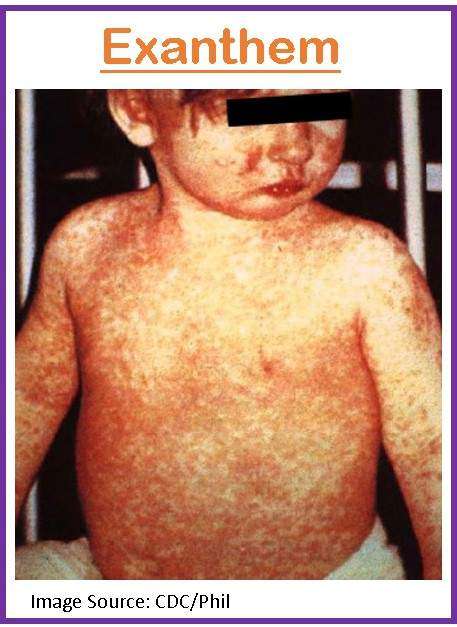
- Exanthem is an eruptive skin rash caused by the infection.
- The characteristic exanthem typically appears 2-4 days after the prodrome and lasts 3-5 days.
- It typically appears 1-2 days after the onset of Koplik spots.
- Mild pruritus may also be present, and the rash typically appears 14 days after exposure, beginning on the face and upper neck and moving down to the extremities.
Pathophysiology of Measles
- Respiratory droplets can be airborne or on surfaces for up to two hours before becoming active and contagious again.
- In tracheal and bronchial epithelial cells, virus replication and initial infection take place locally.
- The measles virus spreads to nearby lymphatic tissues after 2-4 days, possibly through pulmonary macrophages.
- Before the onset of a rash, the measles virus spreads to multiple organs following the amplification of the virus in local lymph nodes. This is called a mainly cell-associated viremia.
- Measles virus infection results in a generalized immune suppression marked by decreases in delayed-type hypersensitivity, interleukin (IL)-12 production, and antigen-specific lymphoproliferative responses that last for weeks to months after the acute infection.
Diagnosis of Measles
The diagnosis is made using a combination of the patient’s symptoms and laboratory tests. Besides history collection and physical examination, the following diagnostic tests are done.
- Antibody Assays: It is the quickest method for confirming IgM antibodies in case of acute measles. Although laboratories can confirm measles by demonstrating more than a 4-fold rise in IgG antibodies between acute and convalescent sera, relying solely on rising IgG titers for the diagnosis delays treatment significantly.
- Viral culture; Urine samples can be sent in a sterile container for viral culture, and nasal and throat swabs can be delivered on a viral transport medium or with a viral culture swab to isolate the virus.
- Reverse transcription polymerase chain reaction (RT-PCR): RT-PCR analysis can be performed to quickly confirm the diagnosis by detecting measles viral RNA in blood, throat, nasopharyngeal, or urine specimens.
- Chest radiography: It should be done if bacterial pneumonia is suspected; the prevalence of measles pneumonia, even in simple cases, reduces the predictive value of chest radiography for bacterial bronchopneumonia.
Treatment/Management of Measles
There is no specific therapy available. These signs typically disappear in 7 to 10 days
After being exposed to the virus, several steps can be taken to safeguard people who do not already have immunity to measles.
The mainstay of treatment is supportive care.
- Ibuprofen (Advil) or acetaminophen (Tylenol) to lower the fever.
- Rest to help strengthen your immune system.
- Hydration– The main focus is on maintaining adequate hydration and replacing fluids lost due to emesis or diarrhea.
- Vitamin A Supplemental -vitamin A should be taken into consideration to prevent blindness, especially for youngsters and individuals who exhibit clinical symptoms of vitamin A insufficiency. Depending on the child’s age, the dose is administered orally just once per day for two days.
- 6 months: 50,000 international units (IU)
- 6 to 11 months: 100,000 IU
- ≥ 1 year: 200,000 IU
- A single, age-appropriate dose of vitamin A is administered again two to four weeks later to kids who have clinical symptoms of a vitamin A deficit.
- Antibiotics Therapy– Antibiotics should be used to treat secondary infections (such as otitis media or bacterial pneumonia), and patients with severe complicated illnesses such as encephalomyelitis should be hospitalized for observation and antibiotic treatment as necessary for their clinical status.
- Post-exposure immunization. After 72 hours following exposure to the measles virus, those lacking measles immunity, including babies, may get the measles vaccine to provide protection. If measles still persists, symptoms are typically less severe and last for a shorter period of time.
- Serum immunoglobulin. Serum immunoglobulin can prevent measles or lessen symptoms if administered within six days of exposure to the virus. It is usually recommended for immunocompromised people after the virus exposure like
- Pregnant women
- Nursing mother
- Other immunosuppressant diseases
Complications of Measles
- Dehydration: Vomiting and diarrhea can cause the body to lose too much water.
- Ear infection: A bacterial ear infection is one of the most frequent side effects.
- Croup (laryngotracheobronchitis): An infection of the upper airway affecting the larynx, trachea, and bronchi.
- Pneumonia; A lung infection is common in measles. A particularly deadly variety of pneumonia that occasionally results in mortality can develop in people with compromised immune systems.
- Encephalitis: An inflammation of the brain associated with measles can occur in about 1 in 1,000 patients. After measles, encephalitis may manifest right away or months later. Encephalitis may result in a permanent brain injury.
- Obstetrical issues: It can result in preterm birth, low birth weight, and fetal mortality.
- Subacute sclerosing panencephalitis (SSPE): A fatal disease of the central nervous system caused by measles virus infection acquired earlier in life. It is extremely uncommon.
- Thrombocytopenic purpura: A life-threatening condition that has low platelet counts and is characterized by purple bruise skin due to bleeding under the skin.
Prevention of Measles
Vaccination
- Vaccination is the most effective way to protect yourself and others from measles.
- The measles vaccine is given to children as part of routine vaccination programs.
- Typically, two doses of the vaccine are administered.
- The MMR vaccination, often known as the Mumps, Rubella, and Varicella vaccine, is a combination vaccine that also protects against measles (the MMRV vaccine).
Routine immunization
- Measles, mumps, and rubella are the three diseases it is typically administered as part of a combination vaccine to prevent (MMR). MMR vaccinations for children should be given twice:
- The first dose between 12 and 15 months of age
- The second between 4 and 6 years
- Keep a minimum 4-week gap between dosages.
- Begin administering an additional dose at 6 months of age when there is a high risk of infection (overcrowding, epidemics, malnutrition, infants born to HIV-positive mothers, etc.), then continue with the recommended immunization schedule.
Following-up vaccination
- When a child under the age of 15 who has missed either one or both doses of a standard immunization is in contact with medical services, they should be immunized.
Other Preventive Measures
- Maintain good hand hygiene after using the restroom, before touching your face, mouth, or nose, and before eating, wash your hands.
- Avoid sharing personal belongings with anyone who might be ill. These can include things like eating utensils, glasses, and toothbrushes.
- Refrain from interacting with sick people.
- Avoid interacting with those who may be more susceptible to illness, such as infants who are too young to receive vaccinations and those with impaired immune systems.
- If you need to cough or sneeze, cover your mouth and nose. Any used tissues should be disposed of right away.
- Make sure to regularly wash your hands and sanitize any surfaces or things that you touch frequently.
Prognosis
- Measles has a typically favorable prognosis, only a small percentage of cases result in death.
- According to the CDC, 0.1-0.2% of children in the United States die from measles each year.
- It is a major contributor to childhood blindness in developing nations, but it can also have a wide range of side effects.
- There is a chance of a poor prognosis, even though many people with measles will recover without any issues.
- Infants and young children under the age of five, individuals over the age of 20, pregnant women, and people with impaired immune systems are more prone to experience serious consequences.
- In the US, mortality is higher in places with poor access to medical care. Vitamin A deficiency and undernutrition may increase the risk of dying young.
- According to the CDC, measles kills between 100,000 and 200,000 people per year throughout the world, mostly from pneumonia or encephalitis.
Summary
- Measles is a highly contagious viral illness that affects mostly children.
- The measles virus spreads quickly and poses a major risk to some individuals.
- Fever, cold-like symptoms, painful, red eyes, and a blotchy rash that lasts for up to a week are some of the symptoms.
- Children who have never received a vaccine and those with compromised immune systems are most at risk of developing serious illnesses.
- Measles complications are frequent.
- Vaccination is the best line of defense against measles.
- Patients have lifetime immunity upon recovery.
References
- Kondamudi, NP., Waymack, JR. (2023, Jan). Measles. StatPearls Publishing, Retrieved on 2023, March22 from https://www.ncbi.nlm.nih.gov/books/NBK448068/
- Moss, W. J. (2017). Measles. The Lancet, 390(10111), 2490–2502. https://doi.org/10.1016/S0140-6736(17)31463-0
- Keller, J. M., Dela Cruz, C. S., Pasnick, S., Gross, J. E., Carlos, W. G., Maves, R., & Jamil, S. (2019). Measles. American journal of respiratory and critical care medicine, 200(1), P1–P2. https://doi.org/10.1164/rccm.2001P1
- Walter, K., & Malani, P. N. (2022). What Is Measles?. JAMA, 328(23), 2370. https://doi.org/10.1001/jama.2022.21363
- Centers for Disease control and Prevention. (2020, Nov 5). Measles (Rubeola). Retrieved on 2023, March 22 from https://www.cdc.gov/measles/index.html
- Nathala, P., Fatima, S., Sumner, R., & Lippmann, S. (2019). Measles 101. Postgraduate medicine, 131(8), 574–575. https://doi.org/10.1080/00325481.2019.1669409
- Chen, H. L., & Tang, R. B. (2020). Measles re-emerges and recommendation of vaccination. Journal of the Chinese Medical Association: JCMA, 83(1), 5–7. https://doi.org/10.1097/JCMA.0000000000000210
- Griffin D. E. (2018). Measles Vaccine. Viral immunology, 31(2), 86–95. https://doi.org/10.1089/vim.2017.0143