Introduction
Enterobiasis, a parasitic condition often known as pinworm or threadworm infection, is caused by a microscopic, white, thread-like worm known as Enterobius vermicularis. It is widespread and mostly affects youngsters. It is very contagious and transfers from one person to another very easily. The illness is particularly common in crowded settings, including schools, daycare centers, and homes with subpar hygiene habits. It is believed that this disease affects millions of people worldwide. Pinworm eggs are minuscule and cannot be seen with the human eye.
It is difficult to eradicate the risk of transmission because they are easy to adhere to surfaces and objects. Even though it typically belongs to a non-serious medical illness, it can be upsetting and uncomfortable. To stop additional infections and reduce the burden of infection on afflicted people and communities, it is crucial to swiftly diagnose and treat sick people. Controlling the infection’s spread requires maintaining adequate personal hygiene and taking precautions against reinfection.
Incidence
- Preschoolers have the second-highest incidence of enterobiasis after school-age children.
- Humans are the only known host; prevalence rates in the general population range from 5–15%; however, they have been on the decline recently; prevalence rates are likely higher in institutionalized individuals, and the infestation rate rises with both population density and personal habits like thumb sucking.
- E. vermicularis infestations are present everywhere and prevalence differs by nation.
- Children under the age of 18, caregivers of infected children, and institutionalized individuals are the categories most prone to contracting pinworms; in these populations, the prevalence can exceed 50%.
- Pinworm illness is thought to impact hundreds of millions of individuals worldwide.
- In some parts of Africa, Asia, and Latin America, the prevalence of enterobiasis has been estimated to be 50% or higher.
Causes of Enterobiasis
The causative parasites for enterobiasis are Enterobius vermicularis. The consumption of pinworm eggs, which are typically found in contaminated surroundings, can lead to enterobiasis.
Risk Factors of Enterobiasis
Several circumstances might enhance the possibility of developing pinworm infection. Among these risk variables are:
Direct contact with a carrier
- Person-to-person contact is the main method of transmitting Enterobiasis.
- One’s likelihood of acquiring the parasite rises if they live with or frequently interact with someone who has pinworms.
Careless hygiene habits
- Enterobiasis risk is increased by improper hand hygiene, such as failing to thoroughly wash hands with soap and water after using the restroom, changing diapers, or handling food.
- Eggs from pinworms can be transferred from contaminated surfaces if basic hygiene is not practiced.
Infectious environments
- Enterobiasis risk is increased in situations with a high incidence of pinworm eggs. This involves residing in neighborhoods with inadequate sanitation, crowded living circumstances, and cleanliness issues.
- If surfaces and items that come into contact with pinworms eggs, such as clothing, towels, bedding, furniture, and toys are not cleaned and disinfected thoroughly, they can become sources of illness.
Age
- Children are more prone to enterobiasis, especially between the ages of 5 and 14.
- This is because they are more likely to share personal goods, engage in close physical contact with others, and occasionally exhibit less developed hygiene habits and awareness.
Institutional settings
- Enterobiasis is frequently observed in institutional settings where there are plenty of children, such as schools, childcare centers, and residential facilities.
Reinfection
- People who have previously had enterobiasis and have not taken the necessary steps to prevent reinfection may be more susceptible to contracting the disease again.
- Reinfection can occur if bed linens aren’t frequently washed and changed, personal hygiene is poor, or if a person comes into contact with contaminated objects or people.
Mode of Transmission of Enterobiasis
Direct person-to-person contact
Direct contact with an infected person is the most typical way of disease transmission. It can happen when people touch or are near the infected individual.
Infected surfaces and items
Pinworm eggs can usually survive up to a few weeks outside the human body. Pinworm eggs can spread if an infected person touches certain items like bedding, clothing, towels, toys, furniture, bathroom fixtures, etc., and surfaces, then later an uninfected individual comes into contact with these contaminated surfaces or things then touches their lips or consumes the eggs, could become ill.
Transmission through air
There is a chance that pinworm eggs could be transmitted through the air, although this happens less often. It can happen after shaking or disturbing contaminated bedding or clothing causes eggs to become airborne. These airborne particles can infect those who breathe them in or consume them.
Indirect transmission by food, water, or soil
Although it occurs less often, pinworm eggs can also be consumed through tainted food, water, or soil. Food may get infected if it is cooked or handled by someone with contaminated hands or if it is cultivated in soil that contains pinworm eggs.
Signs and Symptoms of Enterobiasis
Enterobiasis symptoms and indicators can differ from person to person. Some infected people might not show any symptoms at all, while others might show the following symptoms:
- Anal itching: The most typical sign of enterobiasis is itching around the anus. The pinworm females frequently lay their eggs in the perianal region at night, which makes the itching worse. Intense and ongoing itching can cause discomfort and sleep disruptions.
- Restlessness and trouble falling asleep: The pinworms’ itching can induce restlessness and trouble falling asleep, especially at night. This is a result of the female worms’ enhanced nighttime activity in the anal region.
- Irritability and behavioral changes: Some infected people, particularly youngsters, may display irritability, mood swings, and/or behavioral changes.
- A slight stomach ache or discomfort: Enterobiasis occasionally results in slight abdominal pain or discomfort. In rare cases, intense abdominal discomfort can mimic acute appendicitis.
- Loss of appetite: Infected people may suffer a decreased appetite, which results in a decreased desire to consume.
- Erythema: Patients frequently experience erythema or excoriation of the perineum, vulvae, or both.
- A visual worm sighting
Pathophysiology of Enterobiasis
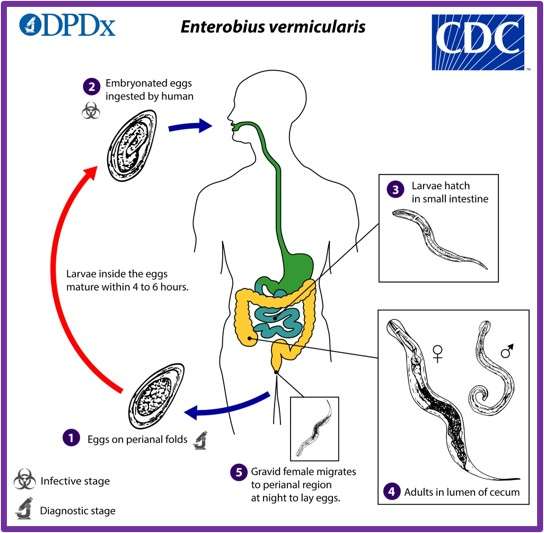
The infection begins after the pinworm eggs are ingested. These tiny eggs are typically found on contaminated surfaces such as bedding, clothing, toys, or other items. Additionally, they can be discovered in food, water, or soil that has been contaminated with feces that contain pinworm eggs. After being consumed, the pinworm eggs hatch in the small intestine. The larvae move on to the large intestine, where they continue to grow and eventually become adult worms. Although the precise mechanism of migration is not entirely understood, it is thought to entail movements made possible by the intestines’ peristaltic contractions.
The larvae develop into adult male and female pinworms in the large intestine. The female pinworms are longer, reaching lengths of up to 8 to 13 mm, while the males are smaller, measuring between 2 and 5 mm. The male pinworms fertilize the females during mating, which takes place in the large intestine. The female pinworms move to the perianal area, or the region surrounding the anus, after mating. When the sick person is asleep at night, this usually happens.
To lay their eggs in the perianal folds, the female pinworms exit from the anus. They lay thousands of eggs in sticky material near the perianal area. Intense itching and discomfort may result from this treatment, especially at night. The scratching that results from the itching might contaminate the fingers and spread the pinworm eggs further.
After being consumed by a new host, the pinworm eggs go through the digestive system before hatching in the small intestine. The cycle continues when the larvae get to the large intestine and develop there into adult worms.
Diagnosis of Enterobiasis
Enterobiasis is normally diagnosed using a combination of clinical assessment and laboratory studies. The primary techniques for diagnosing enterobiasis are listed below:
History and physical examination
A thorough history and inquiring about
- Symptoms include itchiness around the anus, agitation, and trouble falling asleep
- Any risk factors or potential exposure to infected people.
The medical professional may check the perianal region during the physical examination for evidence of pinworms or scratching.
Scotch tape test
The most popular method for identifying enterobiasis is the scotch tape test. It entails taking a sample from the perianal area using clear adhesive tape. Since pinworms are more active at night, this is typically done in the morning before taking a bath or using the restroom. The skin around the anus is touched by the tape, which is subsequently transferred onto a microscope surface. Pinworm eggs, which are minuscule and have a distinctive look, are identified on the slide using a microscope.
Visual examination
Pinworms may occasionally be seen in stool samples or the area around the anus. A medical professional may conduct a visual examination to see the adult worms or their eggs up close.
Stool examination
In some circumstances, a stool sample may be taken and tested to see if pinworm eggs are present. The scotch tape test, however, is typically favored over a stool examination because it has a higher sensitivity for detecting pinworm infections.
Treatment/Management of Enterobiasis
Anthelmintic drugs are the mainstay of treatment for enterobiasis, or pinworm infection. These drugs function by eradicating intestinal pinworms. The treatment’s specifics are as follows:
Mebendazole
- For adults and children older than two years old, a single oral dose of 100 mg of mebendazole is typically prescribed, ideally with food.
- In some circumstances, a second dose may be advised after two weeks to eradicate the infection.
Albendazole
- For adults and children over the age of two, the usual albendazole dosage of 400 mg is administered orally.
- To maximize its absorption, albendazole is typically taken as a single dose with a fatty meal.
- Albendazole may occasionally need to be taken a second dose after two weeks, just as mebendazole.
Pyrantel pamoate
- The usual pyrantel pamoate dosage is determined by body weight. Typically, a single oral dose of 11 mg per kg of body weight, up to a maximum of 1 g, is given.
- Pyrantel pamoate is usually given on an empty stomach, followed by a small meal or snack 1-2 hours later.
- In some circumstances, a second dose may be advised after two weeks.
Complications of Enterobiasis
Most people believe enterobiasis to be a minor illness with minimal complications. But occasionally, certain issues may come up. Here are some potential enterobiasis complications:
Subsequent bacterial infections
- Skin breakdowns might result from scratching the perianal region repeatedly because of the severe itching brought on by pinworm infection.
- It is possible for bacteria to infiltrate through these breaks and spread secondary bacterial illnesses like Cellulitis, impetigo, and streptococcal infection in the perianal region.
Female vulvovaginitis
- In some circumstances, female pinworms may migrate into the female genital canal, causing inflammation and irritation of the vulva and vagina.
- Vulvovaginitis is a disorder that can lead to discomfort, redness, and itching in the vagina.
Appendicitis
- Although it is uncommon, severe pinworm infections can result in appendix inflammation, which is known as appendicitis.
- Pinworms can cause obstruction and subsequent inflammation in the appendix, which may necessitate surgical surgery.
Prevention of Enterobiasis
Enterobiasis risk is significantly lowered by prevention. Here are some crucial preventive steps:
Personal care
- Encourage regular and thorough hand washing with soap and water, especially right after using the restroom, changing a baby, or handling any food.
- Maintain clean, short fingernails to reduce the possibility of pinworm eggs being lodged under them.
Environmental sanitation
- Clean and disinfect surfaces and items regularly throughout the home, especially those in the bathroom and bedroom.
- Examine bedding, towels, clothing, and toys carefully for any potential contact with the perianal area.
- Use a vacuum with a HEPA filter to get rid of pinworm eggs from upholstered furniture, carpets, and rugs.
- Tell people not to share their towels, clothes, or beds because doing so can help spread pinworm eggs.
Knowledge and awareness
- Inform people and their families about enterobiasis, how it spreads, and how to avoid getting it.
- Stress the value of maintaining good personal hygiene habits, such as washing hands, taking regular baths, and maintaining neat fingernails.
- Educate patients on the proper administration of medications and the significance of treating the entire household at once.
Care for afflicted people and close contacts
- Treat everyone at once if one person has enterobiasis, even if none of the household members or close contacts exhibit symptoms. It lessens the chance of infection and spread.
Avoidance of risky situations
- Use extra precautions in places like schools, daycare facilities, and institutions where pinworm illness is more common. These could involve quick detection and treatment of infected people, routine cleaning and disinfection of communal areas, and teaching staff and students about preventative measures.
Prognosis
- Enterobiasis has a good prognosis in most cases.
- The illness can be successfully managed and eradicated with the right care and observance of precautions.
- The cure rate is frequently high with compliance with anthelmintic drugs and in conjunction with good hygiene habits.
- Enterobiasis can reoccur even though treatment is typically effective.
- A moderate illness with few consequences is often thought to be enterobiasis.
- However, continual scratching of the perianal region might result in secondary bacterial infections or skin irritability.
- The appendix or the female vaginal tract may become inflamed in rare cases when the infection is severe.
Summary
The widespread parasitic disease enterobiasis is brought on by the roundworm Enterobius vermicularis. Pinworm eggs are ingested, usually through infected hands or objects, and lead to enterobiasis. Although It is a worldwide infection, congested areas are where it is more common. The main sign of enterobiasis is severe itching around the anus, especially at night. Ingested pinworm eggs spread the highly contagious disease enterobiasis.
The Scotch tape test is helpful for the diagnosis of enterobiasis. Anthelmintic drugs are the mainstay of enterobiasis treatment. Additionally, good personal hygiene, a clean environment, and knowledge of preventative actions are crucial. The prognosis for enterobiasis is good.
Read Also:
- Malaria: Causes, Symptoms, Prevention
- Ascariasis: Causes, Treatment, Prevention
- Filariasis (Lymphatic Filariasis/Elephantiasis)
- Trombiculosis (Chigger Infestation)
References
- Rawla, P., & Sharma, S. (2022). Enterobius Vermicularis. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/30725659/
- Wendt, S., Trawinski, H., Schubert, S., Rodloff, A. C., Mössner, J., & Lübbert, C. (2019). The Diagnosis and Treatment of Pinworm Infection. Deutsches Arzteblatt international, 116(13), 213–219. https://doi.org/10.3238/arztebl.2019.0213
- De Kostha, Y.B.N.S., Pathirana, S.L., Handunnetti, S.M. et al. (2022). Characterization of antigens of Enterobius vermicularis (pinworm) eggs. Sci Rep 12, 14414. https://doi.org/10.1038/s41598-022-18303-8
- Chai, J. Y., Jung, B. K., & Hong, S. J. (2021). Albendazole and Mebendazole as Anti-Parasitic and Anti-Cancer Agents: an Update. The Korean journal of parasitology, 59(3), 189–225. https://doi.org/10.3347/kjp.2021.59.3.189
- Al-Shouli, S. T., Barry, M., Binkhamis, K., AlHogail, N., Alafaleq, N. O., Dufailu, O. A., & Aljerian, K. (2023). Fatal Case of a Child Harboring Enterobius vermicularis. Healthcare (Basel, Switzerland), 11(6). https://doi.org/10.3390/healthcare11060917
- Ummarino, A., Caputo, M., Tucci, F. A., Pezzicoli, G., Piepoli, A., Gentile, A., Latiano, T., Panza, A., Calà, N., Ceglia, A. P., Pistoio, G., Troiano, V., Pucatti, M., Latiano, A., Andriulli, A., Tucci, A., & Palmieri, O. (2022). A PCR-based method for the diagnosis of Enterobius vermicularis in stool samples, specifically designed for clinical application. Frontiers in Microbiology, 13, 1028988. https://doi.org/10.3389/fmicb.2022.1028988
- Centers for Diseases Control and Prevention (2023, June 5). Enterobiasis. Retrieved on 2023 June 12 from https://www.cdc.gov/parasites/pinworm/index.html